At Discover Recovery, your first month is structured, compassionate, and personalized. From the initial phone call to your transition plan, we make sure you know what to expect, why each step matters, and how it supports long-term recovery. This guide walks you through the first 30 days so you can feel informed and ready.
Day 1: Admissions and orientation
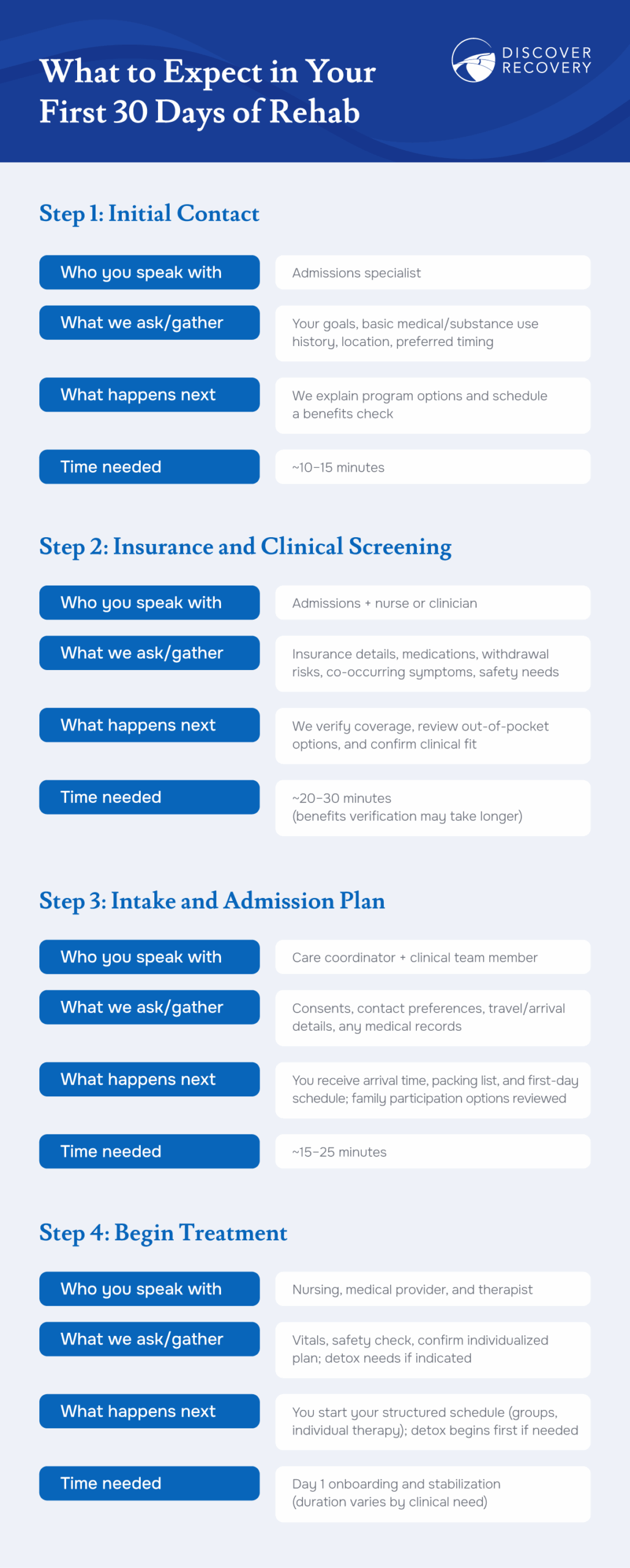
Reaching out for help begins a simple, supportive intake process. When you contact Discover Recovery, an admissions specialist listens to your goals, gathers essential history, and helps you decide which program is the best fit. We discuss how different treatment programs work, from medical detox and residential care to step-down options, so you can choose the right path. We verify insurance benefits and discuss out-of-pocket options so you understand costs before admission. If you have questions about insurance coverage, our team can explain how deductibles, copays, and pre-authorizations work and provide a written estimate.
When you arrive on campus, you complete a comprehensive intake. We will ask about your medical history, substance use history, and mental health conditions. Because substance use and mental health concerns often overlap, screening for co-occurring disorders happens on day one.
You’ll tour the rehab center and meet with members of your multidisciplinary care team—nursing, medical providers, therapists—to begin building a personalized treatment plan. Orientation covers your room and shared spaces, daily routines, safety guidelines, and how to stay in touch with loved ones. Day one balances rest with gentle introductions to the schedule so you can settle in.
Honesty during the intake process matters. Clear, accurate information helps your team tailor medication needs, therapy frequency, and safety planning. The goal is to make your first weeks effective and as comfortable as possible while protecting your health.
Week 1: Detox and stabilization
If appropriate, you begin a medically supervised detoxification process with round-the-clock support to manage withdrawal symptoms.
What the process looks like
Detox includes frequent vital checks, medical monitoring, and appropriate comfort measures. When indicated, clinicians may use medications to ease symptoms, reduce risk, and support sleep and hydration. Nutrition, rest, and calm, consistent support help your nervous system recover from acute stress.
Common symptoms and how they are managed
Depending on your history and substances used, withdrawal symptoms can include anxiety, insomnia, tremors, and mood changes. Your team checks in regularly, adjusts medications when appropriate, and offers grounding techniques and supportive counseling. Alcohol and benzodiazepine withdrawal can be serious; medical supervision reduces complications and provides a safe bridge into the therapeutic process.
How long detox lasts
Many clients complete detox in three to seven days, though timelines vary based on substance use, dose, duration, and overall health. Your plan is adjusted daily until you’re stable enough to step fully into support groups, individual counseling, and wellness activities.
Where medication-assisted treatment (MAT) fits
For certain substance use disorders, FDA-approved medications can be part of care. Examples include buprenorphine for opioid use disorder, and naltrexone, acamprosate, or disulfiram for alcohol addiction treatment. Your team will explain options, benefits, and risks and, if appropriate, integrate MAT with therapy, skills practice, and relapse-prevention planning. Combining medication with counseling and group therapy often improves retention in care and reduces cravings.
Guidance from the Substance Abuse and Mental Health Services Administration (SAMHSA) informs detox safety standards and monitoring.
Daily structure
A predictable, supportive day reduces decision fatigue and helps you rebuild healthy routines. Structure is a cornerstone of early recovery, and it’s calibrated to your needs as you stabilize.
Morning
Mornings usually begin with self-care, a mindful check-in, and a process group or skills-based block. Depending on your plan, you might focus on developing coping strategies for cravings, doing grounding exercises, or DBT-informed emotion regulation. As you progress, you’ll layer in more targeted work, such as relapse-prevention planning.
Afternoon
Afternoon blocks include individual therapy and group therapy sessions, plus education on routines that protect physical health and sleep. Topics may cover the science of addiction, identifying triggers and early warning signs, building routines, repairing relationships, or developing life skills that support long-term recovery.
Evening
Evenings emphasize reflection and connection: peer support meetings, journaling, wellness or creative activities, and sleep hygiene to support restorative rest. Quiet time is not empty time: it consolidates what you’ve learned and prepares you for the next day’s programs.
Consistent structure supports healthy habits and keeps the recovery process moving forward.
Core therapies
Your treatment plan blends evidence-based therapies with holistic supports and is tailored to your goals, history, and stage of care. Throughout your first 30 days, you’ll explore both individual and group work while practicing practical skills you can use right away.
Individual therapy
One-on-one counseling creates a private space to explore motivation, co-occurring mental health concerns, and personal goals. Your therapist may use behavioral therapy approaches (for example, CBT or DBT-informed work) tailored to treatment for substance use and mood symptoms. Sessions often include values work, strengths identification, and practical planning for your week. As you stabilize, your clinician will adjust session targets to match your progress and prepare you for step-down care.
Group therapy sessions
Group therapy is central in most rehab programs, as it offers structure, feedback, and accountability in a supportive environment. Process groups help you make sense of experiences, reduce shame, and learn from peers facing similar challenges. Skills groups teach relapse-prevention tools, communication strategies, boundary-setting, and problem-solving. Psychoeducational groups deepen understanding of substance use disorder, brain and body recovery, and how routines support healing. Many clients find that group therapy accelerates progress by providing honest reflection and encouragement.
Family therapy and involvement
With your consent, clinicians can facilitate family meetings and education about substance use disorders. Family sessions focus on communication, healthy boundaries, and concrete ways loved ones can support the recovery process at home. For many clients, reintegrating into family life is both a motivation and a stressor. Practicing conversations in session and setting expectations together reduces friction later and supports sustained progress after inpatient treatment ends.
Peer support
Connection is protective. In-house recovery meetings and peer-led support groups help you build relationships that outlast a single level of care. Sharing wins, setbacks, and strategies with others nurtures accountability and hope. As discharge approaches, your team will help you identify community-based meetings and recovery resources so you can carry those connections forward.
Integrated care for co-occurring conditions
Co-occurring mental health conditions are common and treatable. Screening during intake and ongoing evaluation allow your team to address mental health and substance use together, an approach associated with better outcomes and continuity of care. Your individualized treatment plan may include medication management, trauma-informed therapy, or additional supports based on your history and goals.
Approaching day 30: aftercare & transition
The first month lays the foundation; the transition plan sustains a successful recovery journey. As day 30 approaches, your team works with you to right-size next steps based on your progress, risks, home environment, and schedule.
Step-down levels of care
Many clients transition to outpatient treatment, either standard outpatient therapy or an intensive option. Our Portland treatment center offers PHP and IOP to maintain structure while you live at home or in recovery housing. Step-down intensity is matched to clinical need: the more support you need, the more hours you’ll attend each week.
Relapse-prevention planning
You’ll develop a written plan that includes your personal triggers, early-warning signs, and specific coping strategies. Practical steps might include a daily routine, a craving-management plan, accountability check-ins, and crisis contacts. If medication-assisted treatment is part of your plan, we’ll coordinate refills, follow-ups, and provider hand-offs so there are no gaps.
30/60/90-day goals
Clear, achievable goals guide ongoing treatment. Examples include attending a set number of therapy sessions per week, participating in peer support meetings, maintaining medication schedules, building sleep and movement routines, and reconnecting with sober supports. Your clinician will help you set milestones and adjust them as life changes.
Family and social reintegration
Returning home can be both exciting and challenging. You’ll practice boundary-setting, conflict resolution, and communication skills in session. Families receive guidance on how to support your recovery journey without over-functioning and how to respond to stress or setbacks. Your ongoing treatment process may include scheduled family check-ins, shared calendars, or agreements around privacy and support.
Discover Recovery’s approach & quality oversight
Discover Recovery provides a continuum of care that starts with medically supervised detox and residential (inpatient) treatment in Long Beach and Camas, WA. Residential clients often transition to our sober living program for continued grounding and support. Clients at our Camas location often continue with our PHP or IOP services in Portland, OR.
At every stage, care is delivered by a multidisciplinary team grounded in evidence-based practices for substance use disorder and co-occurring mental health conditions. Our luxury rehab facilities feature private or semi-private accommodations and holistic, experiential options such as movement, creative arts, and mindfulness, that enhance engagement and well-being. Throughout your stay, clinical leadership and quality oversight ensure that safety, ethics, and client outcomes guide decision-making.
FAQs
What is a typical day like in rehab?
Expect a structured environment with morning check-ins, group therapy, individual counseling, skills or education blocks, wellness or creative activities, and evening peer support. Built-in quiet time supports rest and reflection so you can integrate what you’ve learned.
Is 30 days enough for drug or alcohol addiction treatment?
Thirty days is a strong start: it allows for stabilization, assessment, and consistent therapeutic work. But recovery is ongoing. Many clients continue care after residential treatment in an intensive outpatient program or standard outpatient therapy. Your team will recommend the right duration based on your progress, risks, and support system.
How long does detox take?
Many detox plans last three to seven days, but timelines vary by substances used, dosage and duration, and overall health. Clinicians monitor symptoms and adjust care until you’re stable enough to participate fully in therapy and skills practice.
What happens when I first arrive at a rehab center?
You complete the intake and assessment process, meet your care team, receive an initial schedule, and, if indicated, begin medically supervised detox. Orientation to the environment, routines, and communication guidelines helps you settle in quickly.
How does outpatient treatment fit into recovery?
After residential care, many clients step down to outpatient rehab to maintain momentum while returning to daily life. Depending on clinical needs, this may include an intensive outpatient program (multiple sessions per week) or weekly individual therapy and groups. The goal is continuity: keeping the structure and support that help you succeed.
Conclusion
Your first 30 days in rehab create a foundation for lasting change: safe stabilization, a personalized treatment plan, and daily practice of new skills. Through individual therapy, group therapy, peer connection, and thoughtful aftercare planning, you’ll leave with clarity, momentum, and a roadmap for what comes next. At Discover Recovery, we meet you where you are, supporting your goals with evidence-based care and a structured, compassionate environment designed for healing.
